Guillaume Assié, M.D., Ph.D., Rossella Libé, M.D., Stéphanie Espiard, M.D., Marthe Rizk-Rabin, Ph.D., Anne Guimier, M.D., Windy Luscap, M.Sc., Olivia Barreau, M.D., Lucile Lefèvre, M.Sc., Mathilde Sibony, M.D., Laurence Guignat, M.D., Stéphanie Rodriguez, M.Sc., Karine Perlemoine, B.S., Fernande René-Corail, B.S., Franck Letourneur, Ph.D., Bilal Trabulsi, M.D., Alix Poussier, M.D., Nathalie Chabbert-Buffet, M.D., Ph.D., Françoise Borson-Chazot, M.D., Ph.D., Lionel Groussin, M.D., Ph.D., Xavier Bertagna, M.D., Constantine A. Stratakis, M.D., Ph.D., Bruno Ragazzon, Ph.D., and Jérôme Bertherat, M.D., Ph.D.
BACKGROUND
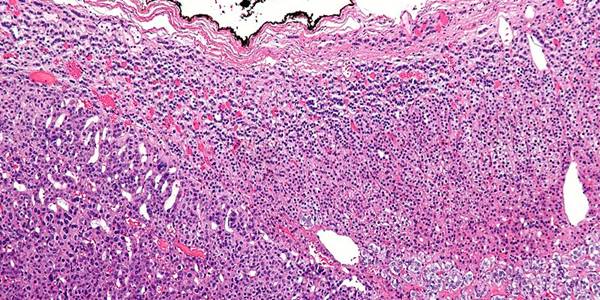
Corticotropin-independent macronodular adrenal hyperplasia may be an incidental finding or it may be identified during evaluation for Cushing’s syndrome. Reports of familial cases and the involvement of both adrenal glands suggest a genetic origin of this condition.
METHODS
We genotyped blood and tumor DNA obtained from 33 patients with corticotropin-independent macronodular adrenal hyperplasia (12 men and 21 women who were 30 to 73 years of age), using single-nucleotide polymorphism arrays, microsatellite markers, and whole-genome and Sanger sequencing. The effects of armadillo repeat containing 5 (ARMC5) inactivation and overexpression were tested in cell-culture models.
RESULTS
The most frequent somatic chromosome alteration was loss of heterozygosity at 16p (in 8 of 33 patients for whom data were available [24%]). The most frequent mutation identified by means of whole-genome sequencing was in ARMC5, located at 16p11.2. ARMC5 mutations were detected in tumors obtained from 18 of 33 patients (55%). In all cases, both alleles of ARMC5 carried mutations: one germline and the other somatic. In 4 patients with a germline ARMC5 mutation, different nodules from the affected adrenals harbored different secondary ARMC5 alterations. Transcriptome-based classification of corticotropin-independent macronodular adrenal hyperplasia indicated that ARMC5 mutations influenced gene expression, since all cases with mutations clustered together. ARMC5 inactivation decreased steroidogenesis in vitro, and its overexpression altered cell survival.
CONCLUSIONS
Some cases of corticotropin-independent macronodular adrenal hyperplasia appear to be genetic, most often with inactivating mutations of ARMC5, a putative tumor-suppressor gene. Genetic testing for this condition, which often has a long and insidious prediagnostic course, might result in earlier identification and better management. (Funded by Agence Nationale de la Recherche and others.)
Supported in part by grants from Agence Nationale de la Recherche (ANR-10-Blan-1136), Corticomedullosurrénale Tumeur Endocrine Network (Programme Hospitalier de Recherche Clinique grant AOM95201), Assistance Publique–Hôpitaux de Paris (Clinical Research Center Grant Genhyper P061006), Institut National du Cancer (Recherche Translationelle 2009-RT-02), the Seventh Framework Program of the European Commission (F2-2010-259735), INSERM (Contrat d’Interface, to Dr. Assié), the Conny-Maeva Charitable Foundation, and the intramural program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
Drs. Assié, Libé, Espiard, Rizk-Rabin, Ragazzon, and Bertherat contributed equally to this article.
We thank Drs. J. Chelly and M. Delpech of the cell bank of Cochin Hospital and Dr. B. Terris of the tumor bank of Cochin Hospital for their help in sample collection; Dr. E. Clauser of the oncogenetic unit of Cochin Hospital for help in microsatellite analysis; Drs. J. Guibourdenche and E. Clauser of the hormone biology unit of Cochin Hospital for cortisol assays; Drs. F. Tissier and Pierre Colin for pathological analysis; Anne Audebourg for technical assistance; J. Metral and A. de Reynies of the Cartes d’Identité des Tumeurs program of Ligue Nationale contre le Cancer for help in genomics studies and fruitful discussions; Dr. P. Nietschke of the bioinformatics platforms of Paris Descartes University for helpful discussions; all the members of the Genomics and Signaling of Endocrine Tumors team and of the genomic platform of Cochin Institute for their help in these studies; and the patients and their families, as well as the physicians and staff involved in patient care, for their active participation.
SOURCE INFORMATION
From INSERM Unité 1016, Centre National de la Recherche Scientifique Unité Mixte de Recherche 8104, Institut Cochin (G.A., R.L., S.E., M.R.-R., A.G., W.L., O.B., L.L., S.R., K.P., F.R.-C., F.L., L. Groussin, X.B., B.R., J.B.), Faculté de Médecine Paris Descartes, Université Paris Descartes, Sorbonne Paris Cité (G.A., S.E., A.G., O.B., L.L., M.S., K.P., F.R.-C., L. Groussin, X.B., J.B.), Department of Endocrinology, Referral Center for Rare Adrenal Diseases (G.A., R.L., O.B., L. Guignat, L. Groussin, X.B., J.B.), and Department of Pathology (M.S.), Assistance Publique–Hôpitaux de Paris, Hôpital Cochin, and Unit of Endocrinology, Department of Obstetrics and Gynecology, Hôpital Tenon (N.C.-B.) — all in Paris; Unit of Endocrinology, Centre Hospitalier du Centre Bretagne, Site de Kério, Noyal-Pontivy (B.T.), Unit of Endocrinology, Hôtel Dieu du Creusot, Le Creusot (A.P.), and Department of Endocrinology Lyon-Est, Groupement Hospitalier Est, Bron (F.B.-C.) — all in France; and the Section on Endocrinology and Genetics, Program on Developmental Endocrinology and Genetics and the Pediatric Endocrinology Inter-Institute Training Program, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD (C.A.S.).
Address reprint requests to Dr. Bertherat at Service des Maladies Endocriniennes et Métaboliques, Centre de Référence des Maladies Rares de la Surrénale, Hôpital Cochin, 27 rue du Faubourg St. Jacques, 75014 Paris, France, or at
jerome.bertherat@cch.aphp.fr.

 PDF (106.3 KB)
PDF (106.3 KB)