In the first two newsletters in this series, we discussed the following:
• The endocrine system and how it is composed of glands throughout the body that release hormones (chemical messengers) into the bloodstream or the fluid surrounding cells. These hormones activate receptors and either alter the cell's existing proteins or instruct the cell in the building of new proteins that create actions in the body.
• The importance of the hypothalamus and the pituitary gland and how these two glands control the two adrenal glands--the HPA axis as it is called, and control the thyroid;
• Each adrenal gland has two parts, the adrenal cortex and the adrenal medulla and the purpose of each;
• The symptoms of adrenal problems and how many of them are similar to symptoms created by problems in the thyroid and other endocrine glands;
• The primary purpose of the adrenal glands, and the entire endocrine system, is to keep the body in a balanced condition called homeostasis;
• The purpose of cortisol and the problems created when cortisol levels are too high or too low;
• How the adrenals can create hypoglycemia, where blood sugar levels are lower than normal;
• How the adrenals affect fatigue, insomnia and obesity;
• How the adrenals affect proper hydration of the body.
Here are links to the first two articles in the series. (http://media.novusdetox.com/dependence.php?include=139775, http://media.novusdetox.com/dependence.php?include=139840)
In this newsletter we will look at the tests used to determine adrenal problems and the most common treatments.
TESTS
If you go to most doctors and say that you are suffering from insomnia, fatigue, hypoglycemia, weight gain and other symptoms of adrenal problems and ask for an adrenal test, most doctors will likely tell you that you need to just take this or that pill and go on a diet. This is always true of Radio Medicine Doctors because they just want to turn up the volume and drown out the symptoms and not treat the cause.
If you persist and demand that they test your adrenals, then they likely will do tests to determine if you have Addison's disease or Cushing's syndrome—diseases where you either have the lowest or highest amounts of cortisol.
First, we will look at the worst cases of adrenal problems and then the more common adrenal problems that affect the majority of us to a greater or lesser extent.
ADDISON'S DISEASE
Addison's disease occurs when the adrenal glands do not produce enough cortisol and, in some cases, aldosterone. This disease is also called adrenal insufficiency, hypoadrenia (“hypo”=low and “ism” =condition of) or hypocortisolism.
According to the National Institute of Health:
• Addison's disease affects about 1 in 100,000 people;
• Adrenal insufficiency occurs when at least 90 percent of the adrenal cortex has been destroyed and no cortisol is being produced.
ADDISON'S DISEASE TESTS
Two of the common tests used to diagnose Addison's disease are:
• ACTH Stimulation Test - where ACTH is released by the pituitary gland to signal the adrenals to produce more cortisol. The ACTH Test usually measures the levels of blood cortisol, urine cortisol before and after a synthetic form of ACTH is given by injection. If the adrenals are functioning properly, there is an increase in blood and urine cortisol levels and the amount of the increase tells doctors about the extent of the adrenal problem.
• CRH Stimulation Test - if the ACTH test is abnormal, a CRH (cortisol releasing hormone from the hypothalamus) stimulation test is used to determine the cause of adrenal insufficiency. Synthetic CRH is injected intravenously and blood cortisol is measured before and 30, 60, 90, and 120 minutes after the injection. If there is no ACTH response, this indicates the problem may be the pituitary gland. If there is a delayed ACTH response, the hypothalamus may be the cause.
ADDISON'S DISEASE TREATMENT
Treatment of Addison's disease requires replacement of the missing cortisol or replacement of the missing aldosterone.
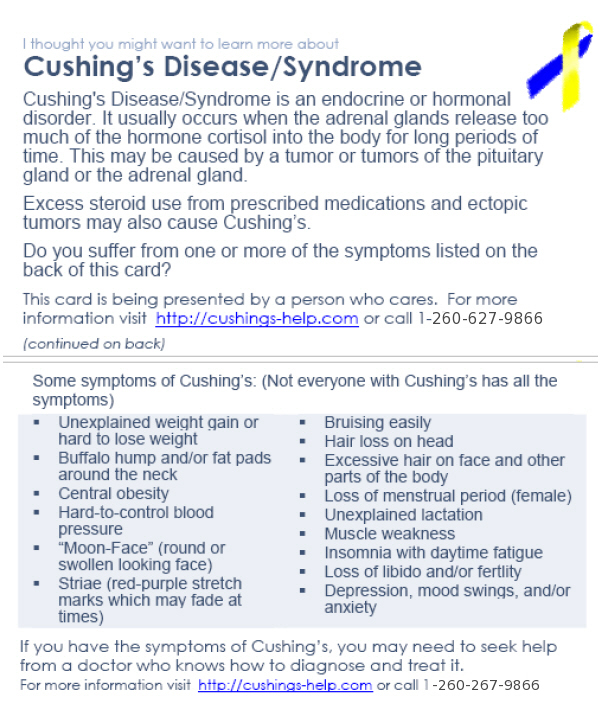
CUSHING’S SYNDROME
Cushing’s syndrome or hypercortisolism (“hyper”=high and “ism” =condition of) is diagnosed when there is a high level of cortisol for a long period of time. According to the National Institute of Health, Cushing’s syndrome is relatively rare and most commonly affects:
• Adults aged 20 to 50;
• People who are obese and have type 2 diabetes.
Because of the dangerous effects of elevated cortisol levels, this is why people who take prednisone (a synthetic form of cortisone that is used in the treatment of rheumatoid arthritis and other inflammatory diseases) or any other form of cortisol should carefully monitor their cortisol levels.
CUSHING’S SYNDROME TESTS
Some of the common tests used to diagnose Cushing’s syndrome are:
• 24-hour urinary free cortisol test where urine is collected over a 24 hour period and tested for cortisol;
• Measurement of midnight plasma cortisol where blood tests to show the level of cortisol at night (when it should be lower at midnight)
• Late-night salivary cortisol where a saliva test is used to determine the level of cortisol at night;
• Giving high or low doses of synthetic cortisol and then checking the urine to see if there is a drop in blood and urine cortisol levels;
• CRH stimulation test described above.
Cushing’s Syndrome Treatment
While the treatment will depend on the cause for the high cortisol levels, some of the traditional options are:
• Surgery;
• Radiation
• Chemotherapy;
• Cortisol-inhibiting drugs.
ADRENAL FATIGUE
As we have learned, your adrenals can be causing problems but you do not have Addison's disease or Cushing's syndrome. Therefore, if you don't have either disease, most doctors don't really address adrenal fatigue—where your adrenals are just not working properly. What if you are experiencing some or all of these symptoms:
• Fatigue
• Have trouble sleeping
• Anxiety
• Sudden weight gain
• Libido is lessened
• Salt cravings
THE SOLUTION--ALTERNATIVE MEDICINE DOCTORS
As we have advised in previous newsletters, it is recommended that you find a doctor who will actually spend the time to find out the physiological cause of your symptoms and treat them. Since the symptoms listed above can be caused by problems with other glands, the doctor will likely have you do a complete set of tests on your most important hormones.
SALIVA CORTISOL TEST
This test measures the cortisol levels at least four times during the day, because cortisol levels are supposed to be highest in the morning and start declining until about midnight and then start rising again. The person uses a small tube to collect the saliva, marks the time and then at set times during the rest of the day and evening the person again spits in a new tube and marks the time. If the person is feeling more fatigued at certain times of the day, then some doctors will also have the saliva test done when they feel fatigued. The saliva samples are then sent to a lab and the cortisol levels for the testing period are shown.
Using this information, the doctor can then advise you as to whether you have adrenal fatigue.
TREATMENT OF ADRENAL FATIGUE
While many doctors are quick to prescribe drugs to address any type of adrenal problem, most alternative medicine doctors will try to use a non-pharmaceutical approach. Here are some of the things that are outlined in Adrenal Fatigue by Dr. James Wilson:
• Do relaxation exercises
• Adjust your sleeping hours
• Physical exercise
• Change your eating times and habits
◦ 40% raw or lightly cooked vegetables
◦ 30% whole grains
◦ 15% beans, seeds and nuts
◦ 10% animal foods
◦ 5% fruits
• Supplements
◦ Vitamin C
◦ Magnesium (particularly if you crave chocolate)
◦ Vitamin E
◦ B vitamins
◦ Calcium
◦ Fiber
◦ Certain herbs
DR. BRENT AGIN'S TREATMENT FOR ADRENAL FATIGUE
Dr. Agin is Novus Medical Detox Center's medical director. In addition to advising on diet changes and on many of the things recommended by Dr. Wilson, Dr. Agin has developed injectable (intra-muscular) vitamins, minerals and herbs that will help provide the support that the adrenals need to recover. Dr. Agin believes that injecting these supplements directly will ensure that more is actually converted and used by the body. The following are the supplements that Dr. Agin's research has indicated are needed to help the adrenals recover:
Vitamin C – 2,000-4,000 mg per day (supports the adrenals and improves immune function)
B-Complex - which includes the following:
• B5 - (Pantothenic acid) 1,000-1,500 mg per day
• B6 - 50-100 mg daily
• B3 - 75-125 mg daily
• B12 - 200-400 mcg daily
Minerals:
• Chromium
Herbal support:
• Licorice Root (not the candy!)- This is well known for supporting the adrenals. It has calming properties along with an ability to increase endurance and energy. It can be taken as a tea, capsule or liquid(in rare cases if large amounts are ingested it can increase the blood pressure).
• Ashwaganda Root- This is considered an adaptogen. An adaptogen is an herb that will help normalize cortisol levels. If there is too much cortisol, it will lower the level, if the level is too low, it will help to increase it.
• Siberian Ginseng- This root helps to uphold and revive adrenal function along with increasing the body’s resistance to stress and normalizing the metabolism. It has antidepressant properties and promotes calmness and a sense of well being. It has been shown to stimulate antibodies to help fight off viruses and harmful bacteria. It also aids in the absorption of B vitamins. (This root usually helps to normalize blood pressure, but if someone has very high blood pressure, then it would still be best to avoid it.)
• Ginkgo- When the adrenals are under a lot of stress, there is an increase in the number of free radicals and if not neutralized, then there is increased risk to the immune system. Ginkgo is a powerful antioxidant along with other supplements that are believed to help counteract the free radicals.
In some cases, Dr. Agin will prescribe additional injectable supplements. The shots are painless and easy to give to yourself. If you are interested in more data about Dr. Agin's injectable products, please email us.
CONCLUSION
At Novus Medical Detox Center, we are very proud that we help people who have become dependent or addicted to substances like OxyContin, methadone, Vicodin, Percocet, heroin, and psychoactive drugs like Xanax and Zoloft and to people who have become addicted to alcohol.
Please call us if we can help someone that you know.
NOTE: This information is provided for general educational purposes only and is not intended to constitute (i) medical advice or counseling, (ii) the practice of medicine, health care diagnosis or treatment, or (iii) the creation of a physician patient or clinical relationship. If you have or suspect that you have a medical problem or that this information may be useful to you or others, please consult with your health care provider before applying any information from our articles to your personal situation or to the personal situation of others.
FAIR USE NOTICE: This may contain copyrighted (C) material the use of which has not always been specifically authorized by the copyright owner. Such material is made available for educational purposes, to advance understanding of human rights, democracy, scientific, moral, ethical, and social justice issues, etc. It is believed that this constitutes a 'fair use' of any such copyrighted material as provided for in Title 17 U.S.C.
Section 107 of the US Copyright Law. This material is distributed without profit.
Technorati Tags: adrenal glands, endocrine system, fatigue, addison's disease, cushing's syndrome, cortisol,
From http://media.novusdetox.com/dependence.php?include=139924