Contributors
Discussions
Categories
- 17a-OH-Progesterone (1)
- 24-hour urine free cortisol (1)
- 24-hour urine test (3)
- abbreviations (1)
- ABC TV (2)
- abstract (5)
- acne (3)
- acromegaly (4)
- ACTH (18)
- activist (1)
- Addison-Biermer disease (2)
- Addison-Schilder syndrome (2)
- Addison's (5)
- Addison's Disease (72)
- Addison’s disease (1)
- Addisonian anemia (1)
- Addisonian crisis (1)
- adenoma (17)
- adrenal (45)
- adrenal cortex (1)
- Adrenal Crisis (33)
- Adrenal Fatigue (8)
- adrenal glands (84)
- Adrenal Insufficiency (58)
- adrenal medulla (1)
- adrenal vein sampling (1)
- adrenal venous sampling (1)
- adrenal-sparing (1)
- adrenalectomy (25)
- adrenaline (1)
- adrenocortical carcinoma (3)
- Adrenoleukodystrophy (1)
- AI (1)
- aldosterone (10)
- aldosteronism (2)
- Alice (2)
- AMRC5 mutation (1)
- androgen (2)
- anniversary (1)
- anxiety (1)
- app (1)
- appendicitis (1)
- April Fools (1)
- arthritis (3)
- autoimmune (1)
- AVIS (1)
- AVS (1)
- award (1)
- awareness (8)
- BclI polymorphism (1)
- benign (3)
- bilateral (2)
- bios (3)
- birthday (2)
- BLA (5)
- blogger (4)
- blogs (10)
- BlogTalkRadio (2)
- blood (2)
- blood pressure (4)
- blood test (2)
- Blue and Yellow (1)
- body image (1)
- bone loss (1)
- books (1)
- brochures (1)
- bruising (2)
- buffalo hump (1)
- Cabergoline (1)
- CAH (6)
- cancer (5)
- Capitol Hill (1)
- carcinoma (1)
- cardiac (1)
- cardiovascular (1)
- Carney Complex (1)
- celiac (3)
- chat (1)
- childhood (1)
- children (2)
- chronic fatigue (1)
- chronic illness (1)
- Chronocort (1)
- chronotherapy (1)
- circadian rhythm (1)
- Cleveland Clinic (2)
- clinical trial (3)
- clinical trials (2)
- comments (1)
- conference (4)
- conference call (1)
- Congenital adrenal hyperplasia (8)
- Congress (1)
- Conn Syndrome (1)
- Conn's Syndrome (3)
- COR-003 (1)
- Corcept (6)
- Corlux (5)
- CORT 108297 (1)
- cortef (3)
- Cortendo AB (1)
- corticosteroids (2)
- corticotropin (3)
- cortisol (14)
- cortisone (6)
- CRH (3)
- Cushie (2)
- Cushie Bookstore (2)
- CushieWiki (6)
- Cushing's (80)
- Cushing's Awareness Challenge (21)
- Cushing's Awareness Day (9)
- Cushing's Disease (15)
- Cushing's Syndrome (5)
- Cushings Help (11)
- CyberKnife (1)
- cyclic (1)
- depression (4)
- dexamethasone (2)
- dexametnosone (1)
- DHEA (3)
- diabetes (14)
- diabetes mellitus (3)
- diagnosis (1)
- disability (1)
- discussion (1)
- doctors (1)
- Donation (1)
- Dr. Adriana Ioachimescu (1)
- Dr. Alfredo Quinones-Hinojosa (1)
- Dr. Amir Hamrahian (2)
- Dr. Barbara Craven (1)
- Dr. Betul A. Hatipoglu (1)
- Dr. Beverly Biller (1)
- Dr. Daniel Kelly (1)
- Dr. David M. Cook (1)
- Dr. Edward Laws (1)
- Dr. Edward Oldfield (1)
- Dr. Harvey Cushing (1)
- Dr. Harvey Williams Cushing (1)
- Dr. James Findling (1)
- Dr. James Lind (1)
- Dr. Lynette Nieman (1)
- Dr. Maria Fleseriu (1)
- Dr. Nelson Oyesiku (1)
- Dr. Roberto Salvatori (2)
- Dr. Shlomo Melmed (1)
- Dr. Theodore Friedman (4)
- drugs (4)
- e-Patient Dave (1)
- Easter (1)
- ectopic (2)
- electrocardiogram (1)
- emergency (1)
- emergency room (1)
- endocrinologist (7)
- endoscopic (2)
- English (1)
- enogenous (1)
- epinephrine (1)
- ER (1)
- exercise (1)
- exophthalmos (1)
- familial (2)
- FAQ (2)
- fatigue (4)
- FDA (4)
- fibromyalgia (1)
- FIPA (1)
- forums (3)
- G-allele (1)
- ganglioneuroma (1)
- genetic (1)
- gland (1)
- Global Genes (1)
- glossary (1)
- glucocorticoid (1)
- glucocorticoids (5)
- glucocortoid (1)
- grand rounds (1)
- Graves' (1)
- Graves' Disease (1)
- Growth Hormone (4)
- haemochromatosis (2)
- Health Activist (1)
- Health Activist Hero award (1)
- Help Wanted (1)
- Helpful Hints (2)
- hemangioma (1)
- hemodialysis (1)
- hGH (2)
- hirsuitism (5)
- holiday (4)
- hormone (1)
- hormones (1)
- HPA axis (4)
- hydrocortisone (3)
- hyperaldosteronism (1)
- hypercortisolism (6)
- hyperkalemia (1)
- hyperplasia (1)
- hyperprolactinemia (1)
- hypertension (2)
- hyperthryoidism (1)
- hypopituitarism (1)
- hypothalamus (1)
- In Memory (3)
- incidentaloma (3)
- infertility (2)
- injection (1)
- insulin (2)
- Insulin Resistance (5)
- Insulin Tolerance Test (1)
- Interviews (7)
- iPad (1)
- iPhone (1)
- IPSS (4)
- Jane Austen (3)
- JFK (7)
- John Kennedy (8)
- Johns Hopkins (4)
- ketoconazole (6)
- kidney (2)
- kidney cancer (1)
- Korlym (11)
- laparoscopic (10)
- levothyroxine (1)
- libido (1)
- Lifetime TV (1)
- liver (1)
- Magic Foundation (1)
- map (1)
- Mary O'Connor (1)
- MaryO (7)
- Mayo Clinic (1)
- media (1)
- Medic Alert ID (1)
- Medical History (4)
- meds (1)
- meeting (2)
- MEN1 (2)
- MEN4 (1)
- message boards (4)
- metyrapone (1)
- midline incision (1)
- Mifepristone (5)
- mitotane (1)
- moon face (1)
- mortality (1)
- MRI (6)
- myelolipoma (1)
- Mystery Diagnosis (1)
- National Women's Health (1)
- Nelson's (1)
- Nelson's Syndrome (1)
- neurosteroids (1)
- neurosurgeon (1)
- News (1)
- news items (2)
- NIH (11)
- noradrenaline (1)
- noripinephrine (1)
- NormoCort (1)
- obese (1)
- obesity (7)
- ophthalmologist (1)
- Oprah (1)
- orphan disease (1)
- osteoporosis (3)
- Pasireotide (3)
- PCOS (3)
- perioperative (1)
- pernicious anemia (2)
- PharmaForm (1)
- pheochromocytoma (13)
- pituitary (52)
- Plenadren® (1)
- PMS (1)
- Podcast (7)
- potassium (3)
- Power Surge (3)
- PPNAD (1)
- prednisone (1)
- pregnancy (2)
- prevention (1)
- primary care (1)
- prizes (1)
- progesterone (1)
- prolactinoma (4)
- Psalm 116 (1)
- pseudocyst (1)
- psoriasis (1)
- quality of life (2)
- R-roscovitine (1)
- radiation (2)
- Rare Disease Congressional Caucus (1)
- Rare Disease Day (1)
- Rare Diseases (4)
- recurrence (2)
- renal artery (1)
- renal cell carcinoma (1)
- resolutions (1)
- retroperitoneal (1)
- ribbons (2)
- Robin (1)
- RSS feed (1)
- salivary (1)
- salivary cortisol (1)
- SEISMIC trial (1)
- Signifor (1)
- SILS (1)
- Sjogren's (1)
- sleep disturbance (1)
- Solu-Cortef (3)
- Spanish (1)
- Spironolactone (1)
- stereotactic (1)
- steroid (2)
- steroids (2)
- straie (4)
- stress (4)
- stretch marks (4)
- stroke (1)
- support (4)
- surgery (25)
- survey (1)
- symptoms (6)
- television (1)
- teriparatide (1)
- testing (4)
- Thankfulness (1)
- Thanksgiving (2)
- The Balancing Act (1)
- The Coffee Klatch (1)
- Thomas Addison (6)
- thyroid (12)
- topical steroid use (1)
- transsphenoidal (8)
- treatment (3)
- TSH (1)
- tumor (13)
- TV (1)
- Twitter (1)
- UFC (2)
- unilateral adrenalectomy (2)
- upgrade (1)
- video (10)
- Vitamin B12 deficiency (1)
- WEGO (1)
- weight (10)
- Wiki (1)
- X-ray (1)
- zebra (1)
- zebrafish (1)
I cannot imagine this myself, since Cushing's is so hard to diagnose but an article at yourdailyjournal.com claims:
The blood profiles provide a comprehensive look at several physiological systems in the body at a cost that is very reasonable for the patients, all in one panel,” Laboratory Manager Rhonda Outlaw said. “The cost savings would amount to anywhere from $185 to $1,100, depending on the tests done and whether they were drawn at a physician’s office or on an outpatient basis.
“The panel itself will give indication of possible problems with kidney functions, hematological functions, like anemia, platelet function and infection; cardiovascular disease, thyroid functions, diabetes detection, liver functions and electrolyte function, like Cushings Syndrome, potassium regulation and dehydration detection.”
What do you think about this?
I would be remiss if I didn't use today's Challenge post to remind readers that there is a wonderful opportunity to ask Dr. Theodore Friedman questions about thyroid or other issues. Dr. Friedman (or Dr. F, as he is called on the boards) has been a help to so many Cushies. He specializes in cyclical Cushing's and seems to be able to diagnose what other, lesser, doctors cannot.
According to his website, goodhormonehealth.com:
So many of us believe that fatigue, weight gain, loss of libido and other problems are just symptoms we must learn to live with. What if these symptoms are not the result of stress, diet, or aging, but are actually caused by a hormonal disorder? Symptoms of hormone deficiency or excess may be subtle and difficult to diagnose. Many hormonal problems are misdiagnosed as depression, especially in women.
You know your own body better than anyone else, and you know when something is wrong. Dr. Friedman is a compassionate, caring physician who will listen carefully to your concerns and work with you to establish a treatment plan. As an experienced, board-certified endocrinologist and researcher, he has the capabilities to diagnose and treat even the most difficult hormonal problems.
Dr. Friedman has found that some of his patients suffer from undiagnosed pituitary or adrenal problems. These include many people suffering from Cushing's disease, which can present a baffling array of symptoms and is frequently misdiagnosed. Other patients may have pituitary or adrenal insufficiency, which has numerous symptoms and is equally hard to diagnose. Dr. Friedman is a world expert in these difficult-to-diagnose diseases and he welcomes inquiries from patients and their physicians.
~~~
Dr. Friedman is not a stranger to Cushings Help.
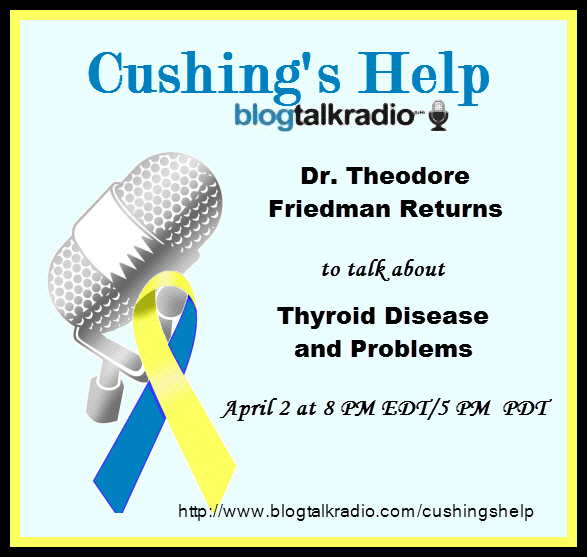
Have questions about thyroid issues?
Ask Dr. Theodore Friedman.
Theodore C. Friedman, M.D., Ph.D. has opened a private practice, specializing in treating patients with adrenal, pituitary, thyroid and fatigue disorders. Dr. Friedman has privileges at Cedars-Sinai Medical Center and Martin Luther King Medical Center. His practice includes detecting and treating hormone imbalances, including hormone replacement therapy. Dr. Friedman is also an expert in diagnosing and treating pituitary disorders, including Cushings disease and syndrome.
Dr. Friedman's career reflects his ongoing quest to better understand and treat endocrine problems. With both medical and research doctoral degrees, he has conducted studies and cared for patients at some of the country's most prestigious institutions, including the University of Michigan, the National Institutes of Health, Cedars-Sinai Medical Center, and UCLA's Charles Drew University of Medicine and Science.
Read Dr. Friedman's First Guest Chat, November 11, 2003.
Read Dr. Friedman's Second Guest Chat, March 2, 2004.
Listen to Dr. Friedman First Live Voice Interview, January 29, 2009.
Listen to Dr. Friedman Second Live Voice Interview, March 12, 2009.
Listen to Dr. Friedman Third Live Voice Interview, February 13, 2011.
Listen to Dr. Friedman Fourth Live Voice Interview, March 12, 2012.
Dr. Friedman will return tonight, April 2, 2012. The call in number with questions or comments is (646) 200-0162.
Listen live at http://www.blogtalkradio.com/cushingshelp
This interview will be archived afterwards at the same link and on iTunes Cushie Podcasts
Ask Dr. Theodore Friedman.
Read Dr. Friedman's Second Guest Chat, March 2, 2004.
Listen to Dr. Friedman Second Live Voice Interview, March 12, 2009.
Listen to Dr. Friedman Third Live Voice Interview, February 13, 2011.
Listen to Dr. Friedman Fourth Live Voice Interview, March 12, 2012.
Labels: Dr. Theodore Friedman, Interviews, Podcast, thyroid
Excerpt from: http://thechart.blogs.cnn.com/2012/02/14/
making-sense-of-your-childs-health-numbers/
"...Unfortunately, as obesity becomes more common among children, diseases once thought to be primarily a problem of adulthood are showing up in kids. For this reason, children should be screened for medical complications of obesity, such as diabetes, high blood pressure and high cholesterol.
Not everyone agrees when you should start screening your children, but the latest recommendation is to test cholesterol between 9 and 11 years old and then again between 17 and 21. Ask your pediatrician for his or her opinion based on your child’s BMI. Blood pressure can be measured with a cuff at the doctor’s office, and diabetes and high cholesterol can be checked with simple blood tests.
These tests may include blood sugar, hemoglobin A1c and insulin levels for diabetes; a lipid panel (such as cholesterol and triglycerides) which, along with blood pressure, is a marker for heart disease; and tests for liver problems that can occur with obesity.
In some situations it might be important to rule out medical causes of obesity. For example, patients who have a higher concentration of fat in the neck and head region could have Cushing's syndrome, and those who are relatively short for their weight and age and have other symptoms might have low thyroid function..."
Read the entire article at http://thechart.blogs.cnn.com/2012/02/14/
making-sense-of-your-childs-health-numbers/
[prMac.com] South Dartmouth, Massachusetts - The Editors of Endotext and Thyroidmanager announce the release of their new medical app, "Endocrinology and Endo Emergency".
The app provides concise, practical information on endocrine emergencies, and provides the answers needed RIGHT NOW for their care. Each of the 36 topics covered includes the clinical recognition, pathophysiology, diagnosis, differential, treatment, and follow up. In addition, references to available Clinical Guidelines, and important literature citations are provided.
Focusing on the critical information needed at the point of care, the app includes topics such as Cushing's disease, diabetic ketoacidosis, managing acute type I and type II diabetes, hypercholesterolemia, adrenal insufficiency, hyperthyroidism, thyroid storm, and much more. Key facts are presented in tables and flow-charts to allow quick reference to crucial information.
The app is designed for physicians, nurses, emergency room caregivers, hospitalists, trainees, students, and any caregiver who needs to treat seriously ill patients.
The "Endocrinology and Endo Emergency" mobile application was created by the world-renowned endocrinologists who also brought you ENDOTEXT.ORG and THYROIDMANAGER.ORG, the most comprehensive and up-to-date web-based endocrine textbooks. Endocrinology and Endo Emergency is always updated with the latest information, and updates can be automatically downloaded by users.
To view or purchase the app in the Apple App store (also available for android) or go to endoemergencies website for information and to view a sample section. Qualified reviewers may contact us for promo codes.
* Covers endocrinology and endocrine emergencies
* Provides critical information needed at the point of care
* 36 topics covered
* written by expert endocrinologists from around the world
Device Requirements:
* iPhone 3GS, iPhone 4, iPhone 4S, iPod touch (3rd generation), iPod touch (4th generation) and iPad
* Requires iOS 5.0 or later
* 1.7 MB
Endocrinology & Endo Emergency 1.0 is $5.99 USD (or equivalent amount in other currencies) and available worldwide exclusively through the App Store in the Medical category.
Endocrine Emergencies
Thyroid Disease Manager
Endotext Web Book
Purchase and Download
Screenshot
App Icon
Produced and owned by Endocrine Education, Inc. and Mdtext.Com, Inc. Copyright (C) 2012 Endocrine Education, Inc. and Mdtext.Com, Inc. All Rights Reserved. Apple, the Apple logo, iPhone, iPod and iPad are registered trademarks of Apple Inc. in the U.S. and/or other countries.
David Unuane, MD (Doctor), Department of Endocrinology, Universitair Ziekenhuis Brussel, UZ Brussel, Vrije Universiteit Brussel, Brussels, Belgium, Herman Tournaye, MD, PhD (Professor, Doctor), Brigitte Velkeniers, MD, PhD (Professor, Doctor), Kris Poppe, MD, PhD (Professor, Doctor)
Female infertility occurs in about 37% of all infertile couples and ovulatory disorders account for more than half of these. The ovaries are in continuous interaction with the other endocrine organs. The interplay may account for infertility occurring at different levels and may render the diagnosis of infertility a difficult exercise for the involved physician. A hypothalamic cause of female infertility should be considered in an appropriate clinical context, with tests pointing to a hypogonadotropic hypogonadism. It can be functional, physiological or related to organic causes. Hyperprolactinemia has well characterized effects on the normal gonadal function and treatment is well established.
Acromegaly and Cushing’s disease may impair fertility at different levels, mechanisms involved however remain ill defined. Thyroid disorders, both hyperthyroidism and hypothyroidism, can interact with the ovaries, through a direct effect on ovarian function, but autoimmunity may be involved, as well as alterations of the sex hormone binding protein levels. Primary ovarian disorders, such as the polycystic ovary syndrome and primary ovarian insufficiency are frequent diseases, for which novel treatments are currently being developed and discussed.
We will propose an algorithm for the diagnosis and approach of the female patient presenting with infertility on the basis of the available evidence in literature.
Keywords: female infertility, pituitary, adrenal, ovarian, thyroid
From http://www.bprcem.com/article/PIIS1521690X1100087X/abstract?rss=yes
Labels: acromegaly, adrenal, Cushing's, hyperprolactinemia, infertility, PCOS, pituitary, thyroid
What Is the Best Approach for the Evaluation and Management of Endocrine Incidentalomas?
Posted by cushie
Key points include: Advances and more frequent use of diagnostic radiology have led to the increased prevalence of endocrine incidentalomas; Pituitary, thyroid, and adrenal incidentalomas must be assessed for dysfunctional hormone secretion and malignant potential; Inpatient management of endocrine incidentalomas should include consultation of endocrine or surgical teams in cases of dysfunctional or malignant lesions; Post-discharge instructions shouldclearly delineate timelines for repeat imaging, laboratory testing, and subspecialist follow-up.
by Darlene Tad-y, MD, Section of Hospital Medicine, University of Colorado Denver

Case
A 54-year-old man with a history of hypertension treated with hydrocholorothiazide and Type 2 diabetes mellitus is admitted with abdominal pain and found to have an incidental 2.1-cm left adrenal mass on CT scan of the abdomen. He denies symptoms of headache, palpitations, weight gain, or muscle weakness. His exam is significant for mildly elevated blood pressure. What is the best approach for evaluation and management of this incidental finding?
Overview
Incidentalomas are mass lesions that are inadvertently discovered during radiolographic diagnostic testing or treatment for other clinical conditions that are unrelated to the incidental mass. In recent decades, improvements in radiographic diagnostic techniques and sensitivity have led to increasing discovery of incidental lesions that are often in the absence of clinical signs or symptoms.1 Three commonly discovered lesions by hospitalists are pituitary, thyroid, and adrenal incidentalomas.2 The concerns associated with these findings relate to the potential for dysfunctional hormone secretion or malignancy.
Patients found with pituitary incidentalomas can be susceptible to several types of adverse outcomes: hormonal hypersecretion, hypopituitarism, neurologic morbidity due to tumor size, and malignancy in rare cases. Thyroid incidentalomas are impalpable nodules discovered in the setting of ultrasound or cross-sectional neck scans, such as positron emission tomography (PET) scans. Discovery of a thyroid incidentaloma raises concern for thyroid malignancy.3 The increased use of abdominal ultrasound, CT scans, and MRI has fueled the growing incidence of adrenal incidentalomas (AIs).
The discovery of an endocrine incidentaloma in the inpatient setting warrants a systematic approach that includes both diagnostic and potentially therapeutic management. A hospitalist should consider an approach that includes (see Table 1):
- Characterization of the incidentaloma, including clinical signs and symptoms, size, hormonal function, and malignant potential;
- Immediate management, including medical versus surgical treatment; and
- Post-discharge management, including monitoring.
Review of the Data
Pituitary incidentalomas. The prevalence of pituitary incidentalomas found by CT ranges from 3.7% to 20%, while the prevalence found by MRI approximates 10%. Autopsy studies have revealed a prevalence ranging from 1.5% to 26.7% for adenomas less than 10 mm, considered to be microadenomas. Broad categories of etiologies should be considered: pituitary adenoma, nonpituitary tumors, vascular lesions, infiltrative disorders, and others (see Table 2). The majority of pituitary adenomas secrete prolactin (30% to 40%) or are nonsecreting (30% to 40%). Adenomas secreting adrenocorticotropin hormone (ACTH, 2% to 10%), growth hormone (GH, 2% to 10%), thyroid-stimulating hormone (TSH, <1%), follicle-stimulating hormone (FSH), and luteinizing hormone (LH) are much less common.2 Significant morbidity and premature mortality are associated with hyperprolactinemia, acromegaly (growth hormone excess), Cushing’s syndrome, and hyperthyroidism. Additionally, up to 41% of patients with macroadenomas were found to have varying degrees of hypopituitarism due to compression of the hypothalamus, the hypothalamic-pituitary stalk, or the pituitary itself.4
TABLE 2. DIFFERENTIAL DIAGNOSIS FOR PITUITARY INCIDENTALOMAS2,4,14
Pituitary adenoma:
- Secreting: prolactin, growth hormone, ACTH, glycopeptides (LH, FSH, TSH, a-subunit)
- Nonsecreting
Non-pituitary tumors:
- Germ cell tumors
- Craniopharyngioma
- Meningioma
- Metastatic disease
Vascular lesions:
- Aneurysms
- Hamartomas
- Infarctions
Infiltrative:
- Sarcoidosis
- Histiocytosis
- Lymphocytic hypophysitis
- Eosinophilic granulomas
Other:
- Rathke’s cleft cyst
- Anatomic abnormalities
ACTH=adrenocorticotropin hormone, GH=growth hormone, TSH=thyroid-stimulating hormone (thyrotropin), LH=luteinizing hormone, FSH=follicle-stimulating hormone
Recently, the Endocrine Society released consensus recommendations to guide the evaluation and treatment of pituitary incidentalomas, which are included in the approach outlined below.5 A detailed history and physical examination should be obtained with specific inquiry as to signs and symptoms of hormonal excess and mass effect from the tumor. Examples of symptoms of hormone excess can include:
- Prolactin: menstrual irregularity, anovulation, infertility, decreased libido, impotence, osteoporosis;
- Growth hormone: high frequency of colonic polyps and colon cancer (chronic excess);
- TSH: thyrotoxicosis, atrial fibrillation; and
- ACTH: hypertension, osteoporosis, accelerated vascular disease.
Symptoms related to the mass effect of the tumor include visual field defects and hypopituitarism related to the deficient hormone, including:
- FSH/LH: oligomenorrhea, decreased libido, infertility;
- TSH: hypothyroidism (weight gain, constipation, cold intolerance);
- ACTH: adrenal insufficiency (hypotension, hypoglycemia, weight loss); and
- ADH: polyuria, polydypsia.
The size and location of the pituitary lesion must be assessed. Lesions greater than 10 mm are considered macroademonas, and their size will affect their management. If the lesion was initially identified by CT scan, an MRI is recommended to better evaluate it.5 If the MRI locates the incidentaloma abutting the optic nerve or chiasm, then the patient should undergo a formal visual field examination.
Indications for an inpatient surgical referral for treatment include: a lesion larger than 2 cm, evidence of mass effect such as visual field defects, neurologic compromise, opthalmoplegia, hypopituitarism, a tumor abutting the optic nerve or chiasm, pituitary apoplexy, and hypersecretion of hormones other than prolactin. Patients with prolactinomas warrant an inpatient endo-crinology consult and may need medical management with a dopamine agonist. Hormone replacement therapy can also be provided for patients with hypopituitarism.2,5
For patients who do not meet the criteria for inpatient surgical therapy, follow-up management must be arranged at the time of discharge. Clinical, laboratory assessment, and an MRI should be scheduled six months after the initial finding of the incidentaloma with the patient’s PCP or with an endocrinologist.5
Thyroid incidentalomas. The prevalence of thyroid nodules based on ultrasound studies ranges from 19% to 46%, with autopsy studies estimating an incidence of approximately 50%.2,6 Incidence of thyroid nodules also increases with age, as almost 60% of people over the age of 60 harbor a thyroid incidentaloma. The rate of malignancy in the general population has ranged between 8% and 24%; however, in the last decade, the rates have increased by 2.4 times as more sophisticated ultrasound techniques and liberal use of fine-needle aspiration (FNA) biopsies have detected subclinical disease.7,8
Etiologies for incidental thyroid nodules can be divided into benign and malignant causes. Benign etiologies include thyroid cyst (simple or complex), multinodular goiter, and Hashimoto’s thryoiditis, while malignant causes include papillary, medullary, follicular, Hurthle cell, and anaplastic carcinomas, thyroid lymphomas, and rare instances of metastatic cancers.2,3
Targeted history and physical examination helps to characterize the thyroid incidentaloma. Historical features, such as palpitations, weight loss, anxiety, new onset atrial fibrillation, or menstrual irregularities, coupled with tachycardia, tremors, proximal muscle weakness, and a palpable nodule aid in the diagnosis of hyperthyroidism. Findings such as a family history of thyroid cancer, symptoms of hoarseness or dysphagia, rapid growth of the nodule, environmental or history of head or neck irradiation along with physical findings of a hard, fixed nodule, or cervical lymphadenopathy increase the suspicion for malignancy.2,7
The functionality of the nodule can be assessed by checking TSH, free T3, and free T4 levels. Suppression of TSH (< 0.1 mU/L) with elevated levels of free T3 and T4 indicates nodule production of excess thyroid hormone and warrants thyroid scintography. Thyroid scintography will identify the nodule as “hot” (hyperfunctioning) or “cold” (nonfunctioning).2
Regardless of the radiographic modality that initially identified the thyroid incidentaloma, a dedicated thyroid high-resolution ultrasound should be ordered to assess the size, multiplicity (single or multinodular), location, and character (solid, cystic, or mixed).7
Recommendations for proceeding to FNA to evaluate for malignancy differ among subspecialty societies. Generally, nodules larger than 1 cm or nodules smaller than 1 cm with risk factors for malignancy should be referred for FNA.2,7
If diagnostic workup identifies a patient with hyperthyroidism due to an autonomously functional nodule or a nodule that may be at high risk for malignancy, it is appropriate to involve an endocrinologist and possibly a surgical subspecialist prior to discharge. Management of hyperthyroidism can include starting antithyroid agents (methimazole or propylthiouracil), radioactive iodine ablation, or referral for surgery.
Preparation for discharge of the patient whose incidentaloma is nonfunctional or does not appear to be malignant should include appointments to recheck thyroid hormone levels, including TSH as well as a thyroid ultrasound within one year of the initial discovery.
Adrenal incidentaloma. The prevalence of AIs found by CT of the abdomen ranges from 0.4% to 4%, while autopsy studies have found a prevalence of 1.4% to 9% with increasing prevalence with age.2,9,10 The majority of AIs are benign and nonfunctioning adenomas, in the absence of known malignancy. Other differential diagnoses include Cushing’s syndrome, pheochromocytoma, adrenocortical adenoma, aldosteronoma, and metastatic lesions.
Because functioning adrenal incidentalomas may be clinically silent, any patient found with an AI must undergo biochemical workup as part of their evaluation to assess for pheochromocytoma, Cushing’s syndrome, and if he or she has a history of hypertension or hyperaldosteronism (Conn’s syndrome). Table 3 outlines the approach for characterizing adrenal incidentalomas.2,11,12 An important point is that imaging studies are not useful in distinguishing a functioning versus nonfunctioning tumor but rather can help to discriminate malignant lesions.11
Inpatient surgical consult for resection is indicated if the patient is found to have pheochromocytoma, clinically apparent functioning adrenocortical adenoma, or a tumor size greater than 4 cm. Consultation with an endocrinologist is also recommended if biochemical tests are positive. If the diagnostic workup leads to suspicion for infection or metastatic disease, the patient should be referred for FNA.2,12
For patients whose lesions do not require surgical resection, repeat CT scan of the abdomen is recommended six months from the initial finding. Hospitalists should also arrange for the patient to repeat biochemical testing, including an overnight dexamethasone test.12,13
Back to the Case
The patient underwent biochemical testing and was found to have normal levels of plasma-free metanephrines, a plasma aldosterone, plasma renin activity ratio less than 20, and a serum cortisol level of 7 mg/dL after his overnight dexamethasone suppression test. The 24-hour urine collection for free cortisol revealed elevated levels of cortisol in the urine, and the ACTH level was low.
Endocrinology and endocrine surgery teams were consulted, and recommended surgical resection. After surgical resection of his tumor, the patient was started on glucocorticoid replacement and was discharged with a follow-up appointment with endocrinology.
Bottom Line
An inpatient approach to endocrine incidentalomas should include characterization of the clinical signs and symptoms, size, function, and malignant potential of the lesion. Based on this, inpatient surgical or medical management can be determined. Post-discharge management should include arrangements for surveillance testing and follow-up with appropriate subspecialists.
Dr. Tad-y is assistant professor of medicine and a hospitalist at the University of Colorado Denver.
KEY POINTS
- Advances and more frequent use of diagnostic radiology have led to the increased prevalence of endocrine incidentalomas.
- Pituitary, thyroid, and adrenal incidentalomas must be assessed for dysfunctional hormone secretion and malignant potential.
- Inpatient management of endocrine incidentalomas should include consultation of endocrine or surgical teams in cases of dysfunctional or malignant lesions.
- Post-discharge instructions should clearly delineate timelines for repeat imaging, laboratory testing, and subspecialist follow-up.
ADDITIONAL READING
- Shirodkar M, Jabbour SA. Endocrine incidentalomas. Int J Clin Pract. 2008; 62:1423-1431.
- Freda PU, Beckers AM, Katznelson L, et al. Pituitary incidentaloma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:894-904.
- Iyer NG, Shaha AR, Silver CE, et al. Thyroid incidentalomas: to treat or not to treat. Eur Arch Otorhinolaryngol. 2010;267:1019-1026.
- Zeiger MA, Siegelman SS, Hamrahian AH. Medical and surgical evaluation and treatment of adrenal incidentalomas. J Clin Endocrinol Metab. 2011;96:2004-2015.
References
- Aron DC, Howlett TA. Pituitary incidentalomas. Endocrinol Metab Clin North Am. 2000;29:205-221.
- Shirodkar M, Jabbour SA. Endocrine incidentalomas. Int J Clin Pract. 2008;62:1423-1431.
- Burguera B, Gharib H. Thyroid incidentalomas. Prevalence, diagnosis, significance, and management.Endocrinol Metab Clin North Am. 2000;29:187-203.
- Molitch ME. Nonfunctioning pituitary tumors and pituitary incidentalomas. Endocrinol Metab Clin North Am. 2008;37:151-171, xi.
- Freda PU, Beckers AM, Katznelson L, et al. Pituitary incidentaloma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:894-904.
- Gough J, Scott-Coombes D, Fausto Palazzo F. Thyroid incidentaloma: an evidence-based assessment of management strategy. World J Surg. 2008;32:1264-1268.
- Iyer NG, Shaha AR, Silver CE, et al. Thyroid incidentalomas: to treat or not to treat. Eur Arch Otorhinolaryngol. 2010;267:1019-1026.
- Jin J, Wilhelm SM, McHenry CR. Incidental thyroid nodule: patterns of diagnosis and rate of malignancy. Am J Surg. 2009;197:320-324.
- Davenport C, Liew L, Doherty B, et al. The prevalence of adrenal incidentaloma in routine clinical practice.Endocrine. 2011;40:80-83.
- Zeiger MA, Siegelman SS, Hamrahian AH. Medical and surgical evaluation and treatment of adrenal incidentalomas. J Clin Endocrinol Metab. 2011;96: 2004-2015.
- Zeiger MA, Thompson GB, Duh QY, et al. American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons Medical Guidelines for the Management of Adrenal Incidentalomas: executive summary of recommendations. Endocr Pract. 2009;15:450-453.
- NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”).NIH Consens State Sci Statements. 2002;19:1-25.
- Young WF. Clinical practice. The incidentally discovered adrenal mass. N Engl J Med. 2007;356:601-610.
- Chidiac RM, Aron DC. Incidentalomas. A disease of modern technology. Endocrinol Metab Clin North Am. 1997;26:233-253.
Addison's disease presenting with idiopathic intracranial hypertension in a 24-year-old woman: a case report
Posted by cushieDushyant Sharma  , Rohini Mukherjee
, Rohini Mukherjee  , Peter Moore
, Peter Moore  and Daniel J Cuthbertson
and Daniel J Cuthbertson 
Journal of Medical Case Reports 2010, 4:60doi:10.1186/1752-1947-4-60
Published:
19 February 2010
Abstract (provisional)
Introduction
Idiopathic intracranial hypertension can rarely be associated with an underlying endocrine disorder such as Cushing's syndrome, hyperthyroidism, or with administration of thyroxine or growth hormone. Though cases of idiopathic intracranial hypertension associated with Addison's disease in children have been reported, there is only one documented case report of this association in adults. We describe a case of an acute adrenal insufficiency precipitated by idiopathic intracranial hypertension in a Caucasian female.
Case presentation
A 24-year-old Caucasian woman was acutely unwell with a background of several months of generalised fatigue and intermittent headaches. She had unremarkable neurological and systemic examination with a normal computerised tomography and magnetic resonance imaging of the brain. Normal cerebrospinal fluid but increased opening pressure at lumbar puncture suggested intracranial hypertension. A flat short synacthen test and raised level of adrenocorticotrophic hormone were consistent with primary adrenal failure.
Conclusion
Addison's disease can remain unrecognised until precipitated by acute stress. This case suggests that idiopathic intracranial hypertension can rarely be associated with Addison's disease and present as an acute illness. Idiopathic intracranial hypertension is possibly related to an increase in the levels of arginine vasopressin peptide in serum and cerebrospinal fluid secondary to a glucocorticoid deficient state.
The complete article is available as a provisional PDF. The fully formatted PDF and HTML versions are in production.
A review of President Kennedy's medical records also shows a family history of autoimmune diseases.
By Susan J. Landers, AMNews staff. Posted Sept. 11, 2009.
New research points to an autoimmune endocrine disorder as the cause of at least some of President John F. Kennedy's health problems.
Despite his relative youth -- at 43, Kennedy remains the youngest person elected president -- and his seeming vigor, Kennedy "had the most complex health history of anyone to occupy the White House," said Lee R. Mandel, MD, MPH, senior medical officer of the aircraft carrier USS George H.W. Bush and a historian interested in presidential medicine. His findings were published in the Sept. 1 Annals of Internal Medicine (www.annals.org/cgi/content/abstract/151/5/350/).
For his study, Dr. Mandel combined evidence gleaned from his review of Kennedy's medical records at the John F. Kennedy Presidential Library and Museum in Boston, with material obtained from additional sleuthing. Kennedy's complex medical history has received much scrutiny since his medical records were made public in 2002.
Dr. Mandel found mentions of Kennedy being diagnosed with hypothyroidism and Addison's disease.
"The fact that Kennedy, who unequivocally had Addison's disease, also had hypothyroidism leads to the plausible conclusion that there was an autoimmune basis for his medical problems, and APS 2 [autoimmune polyendocrine syndrome type 2] explains these conditions," Dr. Mandel wrote.
"I saw the common thread that other people had commented on casually," he said in an interview. "I think he did have an autoimmune syndrome."
Autoimmune thyroid disease coexists with Addison's disease in two-thirds of cases. APS 2 typically occurs in early adulthood, at around age 30, the age Kennedy was when Addison's disease was diagnosed, Dr. Mandel said.
Autoimmune syndromes are often found in families, he added. "[Kennedy's] sister Eunice [Kennedy Shriver], who just passed away, was believed to have Addison's disease and his son, John F. Kennedy Jr., had Graves' disease."
Kennedy also had intestinal ailments likely caused by undiagnosed celiac disease, Dr. Mandel said.
In an era when media scrutiny is less intense than today, Kennedy and his physicians were able to conceal many of his health problems or attribute them to heroic activities. For example, back pain stemming from his degenerative condition was instead attributed to a war injury. Symptoms from his Addison's disease were described as a recurrence of malaria contracted in World War II.
But even if he were running for election today rather than in 1960, Kennedy's Addison's disease would likely not prove an obstacle. Even without modern advances, Kennedy's disease was well-controlled, Dr. Mandel said. He attributed that feat to Kennedy's endocrinologist, Eugene Cohen, MD, "the brains behind the management of the disease."
From http://www.ama-assn.org/amednews/2009/09/07/prsf0911.htm
Labels: Addison's Disease, autoimmune, Graves' Disease, JFK, John Kennedy, thyroid
Good general info for anyone of any age, no matter what symptoms or disease you may have.
by John Beale
Good communication between patients and their health-care practitioners is essential for good care. To help older adults better communicate with their health-care providers, the American Geriatrics Society's Foundation for Health in Aging has released a new, easily understandable tip sheet.
The tip sheet, "How to Talk to Your Healthcare Practitioner: Tips on Improving Patient-Practitioner Communication," outlines steps older adults and their caregivers can take before, during and after a visit to a practitioner. These steps help ensure practitioners, older patients and their caregivers get the information they need. The tip sheet is available online at: http://www.healthinaging.org/public_education/communication_tips.php.
Before visiting a health-care provider, the tip sheet advises older people to, among other things, make a list of any symptoms or health problems they have, as well as past health problems, any treatments they've undergone and any adverse reactions to treatments they have had.
Bring medications
It also encourages older adults to put the medications, supplements and other remedies they're taking in a bag and bring it to their appointment. That way, their practitioner can see what they're taking and at what doses - important information, since medications may interact and some may affect medical test results.
The tip sheet also advises older adults who don't speak English as a first language to consider looking for a practitioner who speaks their native tongue, bring along a bilingual buddy to translate or call the office and request a translator ahead of time.
The tip sheet encourages older patients and their caregivers to answer all questions frankly, to request explanations when needed and to ask follow-up questions, such as "Are there any risks associated with this treatment?" and "Are there any alternative treatments?"
Understanding is vital
It also suggests patients and caregivers repeat back what their providers tell them about their health and treatments to ensure they've understood correctly.
After an appointment, the tip sheet advises older patients to contact their practitioner's office if they don't feel better, if they have an adverse reaction to a medication or other treatment or if they realize they've forgotten to mention something important that's relevant to their health.
Other easy-to-read health tip sheets for older adults and their caregivers cover such topics as cold and immunizations, falls prevention, emergency planning, and joint replacement surgery for older people.
Anyone who does not have online capability may call the Office for the Aging at 845-486-2555 for tip sheet copies.
From http://www.poughkeepsiejournal.com/article/20090629/COLUMNISTS06/906290301/1005/LIFE
~~~
How to Talk to Your Healthcare Practitioner: Tips on Improving Patient-Practitioner Communication
The list mentioned in the article from http://www.healthinaging.org/public_education/communication_tips.php
Good communication between you and your healthcare practitioners -- the physicians, nurse practitioners, nurses, physician assistants and other healthcare professionals you see -- is essential to good care.
It's important that you give your practitioner the information about yourself and your health that he or she needs to provide quality care. And it's important that he or she explain what you need to do to stay as healthy as possible, in a way that you understand.
Here's what experts with the American Geriatrics Society's Foundation for Health in Aging (FHA), suggest:
Before your appointment
Make a list Visiting a healthcare professional can be stressful -- particularly if you're not feeling well -- and stress can make it harder to remember what you need to tell and ask your practitioner. So make a list and bring it to your appointment. Write down any health problems you have had or do have, and any surgery or other treatments you've undergone. Write down the names of any medications you've taken that have caused unpleasant or dangerous side effects. If you're sick, write down all of your symptoms.
And don't forget to write down any questions about your health that you might have. You can find comprehensive lists of questions that older adults should consider asking their healthcare practitioners - organized by subject - on "Aging in the Know" (www.healthinaging.org/agingintheknow/questions_trial.asp), the FHA's free senior health website.
Bring your medications, vitamins, and other remedies to your appointment Before leaving for your visit, put all of the prescription drugs, over-the-counter medications, herbs, vitamins, and other supplements you take in a bag. Take them with you and show them to your healthcare practitioner. This way, he or she will know exactly what you're taking, when, and at what doses. This is important because some drugs, herbs and supplements can interact with medications your practitioner might prescribe. They might also affect the results of certain medical tests.
Pack paper Bring paper or a notebook to your appointment so you can write down what your healthcare professional tells you. If you have trouble remembering later on, you can look at your notes.
Consider asking a buddy along A family member or close friend who goes with you when you see your healthcare professional can offer your practitioner information that you might forget or overlook. He or she can also help you remember what your healthcare practitioner says. If you want to discuss something with your practitioner alone, you can always ask your relative or friend to leave the room while you do so.
Call ahead to request a translator if necessary If English is not your first language, you might seek out a healthcare practitioner who speaks your native language. Other options include bringing a bilingual buddy with you to your appointment, or calling your practitioner's office ahead of time and asking if staff can supply a translator.
During your appointment
Answer questions honestly It's essential that you answer all of the questions your healthcare practitioner asks you, even if he or she asks about topics that might make you uncomfortable, such as mental health problems, drinking, and sex. There's nothing to be embarrassed about. Your practitioner needs complete information to provide proper care. And everything you tell him or her is confidential.
Ask questions If you don't understand what your healthcare professional tells you during your visit, ask him or her to explain it. You need to -- and have a right to -- understand what your practitioner says. It's particularly important that you understand any treatments he or she recommends. You should ask if there are any risks associated with treatments, and if there are any alternatives.
Mention any cultural or religious traditions that might affect your care If your healthcare practitioner recommends that you eat foods that your religion prohibits, for example, or if you need to fast at certain time of the year, tell him or her.
Repeat back After your healthcare professional explains what you should do to stay healthy, or to treat a health problem, repeat this back to him or her using your own words. You might start by saying, "So, you're telling me that I should…." If you've misunderstood his or her advice, your practitioner will realize this, and clarify.
Ask for written instructions If your healthcare practitioner puts his or her advice in writing, you can refer to the written instructions at any time.
After your appointment
Call your practitioner's office if you don't feel better, have a bad reaction to medications, or realize you forgot to mention something If you don't feel better after your visit, or seem to be having a bad reaction to medication your healthcare professional prescribed, call his or her office immediately. You should also call if you realize, after leaving the office, that you neglected to ask a question or provide information about your health, or didn't understand what your healthcare practitioner said. Ask to speak with your practitioner as soon as he or she is available or ask to speak to another healthcare professional in the office who can help you.
Communication between you and your healthcare practitioner is an ongoing process. The simple tips above can help improve communication. Improved communication means better understanding, diagnosis and treatment.
Remember my usual disclaimer!
Honoring an inspiration
Galesburg Register-Mail - Galesburg,IL,USA
By TOM LOEWY Right now she is a 15-year-old girl fighting adrenocortical carcinoma, an aggressive cancer originating in the cortex of the adrenal gland. ...
See all stories on this topic
Pharmacy giving hormone talks
Canada.com - Don Mills,Ontario,Canada
Adrenal Fatigue can often mirror symptoms of menopause. The adrenal gland makes up for other endocrine deficiences in the body and will often become over ...
See all stories on this topic
From Chaos to Consilience
Psychiatric Times - New York,NY,USA
For example, having a tumor in the thyroid complicates understanding of what a pancreatic or adrenal tumor is doing, and vice versa. ...
See all stories on this topic
Aldosterone Provides New Treatment for Age-Related Hearing Loss
Natural News.com - Phoenix,AZ,USA
Aldosterone is a steroid hormone from the mineralocorticoid family, produced in the adrenal cortex. It regulates kidney function and plays a role in ...
See all stories on this topic
Beware of too much potassium
St. Augustine Record - St. Augustine,FL,USA
Nonfunctioning adrenal glands and red blood cells breaking up in the circulation can cause potassium elevation. You can do nothing on your own about these ...
Lower Levels Of Vitamin D Linked To Asthama Severity In Kids
TopNews - Noida,Uttar Pradesh,India
... with augmented hyperreactivity and were likely to have utilized more inhaled adrenal cortical steroids, all symptomatic of higher asthma harshness. ...
Our Tortured Soul
Cornell University The Cornell Daily Sun - Ithaca,NY,USA
Your lungs scream for air, your nerve synapses fire in a panic to the adrenal glands and release a painful adrenaline rush, brutally increasing your heart ...
Life-wise
Wellington Advertiser - Wellington,ON,Canada
The internist explained: "Exercise or tension causes an adrenal rush, which should energize your muscles. But it does the opposite, causing muscles to ...
Community Calendar: Del Mar
Del Mar Times - Del Mar,CA,USA
-Wellness 101 lecture on thyroid and adrenal hormones: 6:45 to 8: 45 pm Stratford Inn, 710 Camino Del Mar. Free. To sign up, call 481-9854 or e-mail ...
Labels: adrenal glands, cortisone, thyroid




